Colorado ERs seeing uptick in serious mental health concerns

In the beginning, COVID-19 scared people from going to emergency rooms, seemingly out of fear of being exposed to the virus.
Now staff in Colorado emergency rooms say people are coming back, often with more serious mental health concerns than before the pandemic.
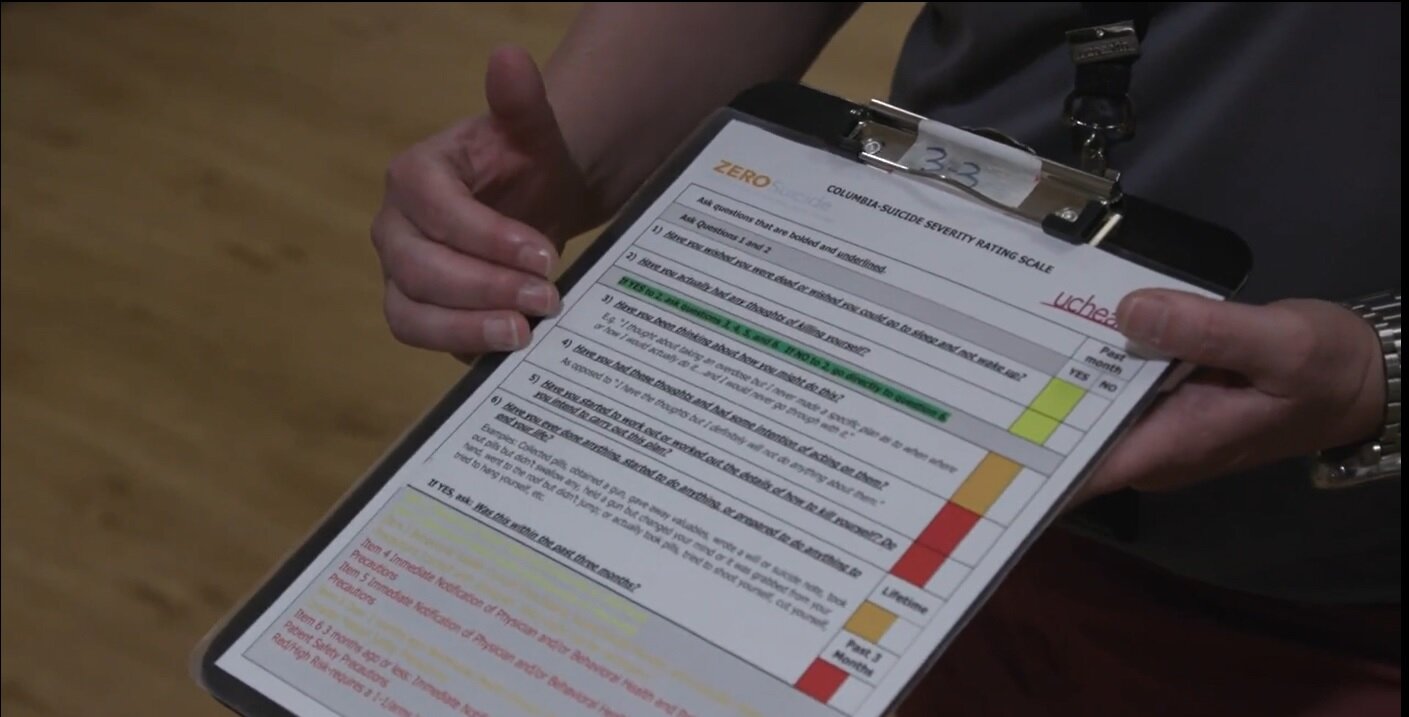
At Memorial, Wood runs the hospital’s Zero Suicide effort, which trains every staff member in the emergency department to screen patients for suicide risk. Even patients who come to the emergency room for physical injuries or a medical emergency that is seemingly unrelated to mental health are screened.
Wood said it’s important for everyone with a loved one who seems to be struggling to ask the question directly: Are you thinking of suicide?
“Talking about it does not cause it. That is absolutely a myth. We have to open the door. We have to start having those discussions,” Wood said.
Ratliff says it is important for people to find ways to stay connected to other people when we are isolated from so many aspects of life we once took for granted.
“If you live in the same area, you can social distance and stay six feet apart and visit grandma ... maybe you stay on the sidewalk, but you wave and you have that connection and you see each other,” Ratliff said. “Use FaceTime, use Skype ... seeing that person on video or in real-time is very important.”
Mental health professionals are also urging people who are struggling during this difficult time to take advantage of the expansion of telehealth options.
“Many of us are going to benefit from support. Folks who haven’t sought support before, it can be tremendously beneficial. The key is it’s available to everyone now, more than ever, safely,” Muir said. “Everyone should have their own mental wellness plan, because everyone’s being impacted across the world. We’ve never had anything like this in my lifetime.”
Resources:
Colorado Crisis Services has a phone line, text line and walk-in clinics available 24/7 around the state. Call 1-844-493-TALK or text “TALK” to 38255.
Porter Adventist Hospital's Behavioral Health Services has a tele-assessment center which can be reached at (303) 715-2300.
Not sure how to start the conversation about mental health? Let’s Talk Colorado has tips.
National Alliance on Mental Illness: COVID-19 Resources
“I think the reason people are coming back is because... it's more than an emergency. Now, it is something they cannot manage on their own any longer,” said Billie Ratliff, director of behavioral health for UCHealth’s southern Colorado region.
Ratliff said UCHealth Memorial Hospital in Colorado Springs saw a decline in behavioral health patients in the final weeks of March and the beginning of April during stay-at-home orders. In the second half of April, patient volume began to increase. Now, Ratliff said July patient numbers approach the regular traffic the emergency room saw before the pandemic -- and patients tended to be more acutely in crisis than before.
“We're seeing an entire spectrum of issues that without the pandemic, I don't think we would have seen. Isolation is very difficult for people,” Ratliff said.
Emergency rooms across the state reported a similar trajectory of behavioral health patients during the COVID-19 pandemic.
A spokesperson for HealthONE said its 12 metro Denver emergency departments have seen a similar pattern in patient volume, and are seeing a slightly larger percentage of patients whose conditions are so acute they require admission to the hospital.
Data gathered by Centura Health showed the number of patients given psychiatric evaluations in its metro Denver emergency rooms in April dropped to 469 from 569 the previous year. At the same time, the percentage of behavioral health patients whose conditions were serious enough to require admission to the hospital grew. Behavioral health patient numbers since then are consistent with pre-pandemic levels.
Andrea Wood evaluates patients for suicide risk at Memorial’s emergency department.
“Probably the biggest thing that we’ve noticed is people who have never had that issue before … people you would look at and never think, because they’re a CEO or they’re a nurse or they’re a physician, [who] never have suicidal thoughts or these kinds of stressors. Those are the people we’re seeing now,” Wood said.
Memorial’s emergency department staff said they are starting to see more children and teenagers coming in with behavioral health concerns.
“They're stressing, they're overwhelmed. They're not sure what's happening. ‘Am I going back to school? Am I not going back to school?’” Wood said. “A lot of kids are at home taking care of their siblings because mom and dad have to go to work. So there's just so many different stressors. But most kids will tell you not being able to engage the way that they normally engage is a very, very stressful and difficult process.”
Children’s Hospital Colorado said its pediatric emergency departments in both Denver and Colorado Springs are not necessarily seeing more patients but are seeing an increase in acute mental health cases.
Staff at Centura Health are particularly alarmed about the patients they are not seeing coming through the doors very often: senior citizens.
“That makes sense because they have significant fears of health and exposure,” said Doug Muir, behavioral health system director for Centura Health. “But getting them linked and supported is really important because we know that they’re the ones most socially isolated by Covid and so they have the greatest need.”
